Depression
February 13, 2022 — September 24, 2022
Suspiciously similar content
Content warning:
Mental health
For most of my life, some people close to me have battled with depression.1 There have been a few cases spiraling chronically out of control. I’m keeping notes of what useful things I learn about managing/assisting/engaging with people afflicted by this condition, in the hope I can apply them in the service of various loved ones in the future.
1 Background
Scott Alexander, Peer Review Request: Depression.
2 Conversing with a depressed person
2.1 Be careful
We all (mostly?) would like to talk to any fellow human with compassion and respect. How do we accomplish this with depressed people? I know that acute trauma definitely has special care requirements. I suspect that depression does too.
Attempting extra compassion for someone who is sad is probably a good idea, regardless of whether that sadness is diagnosable chronic depression or not. Feeling sad, it turns out, is shit.
That said, my fraught and tragic experience in this area indicates that possibly the best way to talk to a depressed person who is sufficiently deep in their illness is with extreme care, and possibly firmly maintained emotional distance. Being actively helpful might require specialised counselling skills, as it involves communicating with someone in a vulnerable state with a compromised ability to communicate their needs.
Also, I would like to know: Which interventions are likely to be helpful, and which not? Which are likely to be most helpful? In a life with finite hours, I want to spend my helping time efficiently. Also, I am not a professional counsellor or psychiatric nurse or social worker, so I want to keep a firm bound on how much I can actually do which is realistic for a non-specialist. Also, presumably the skills of a professional include various important training I do not have, such as not making things worse. What are good bounds on how helpful to be?
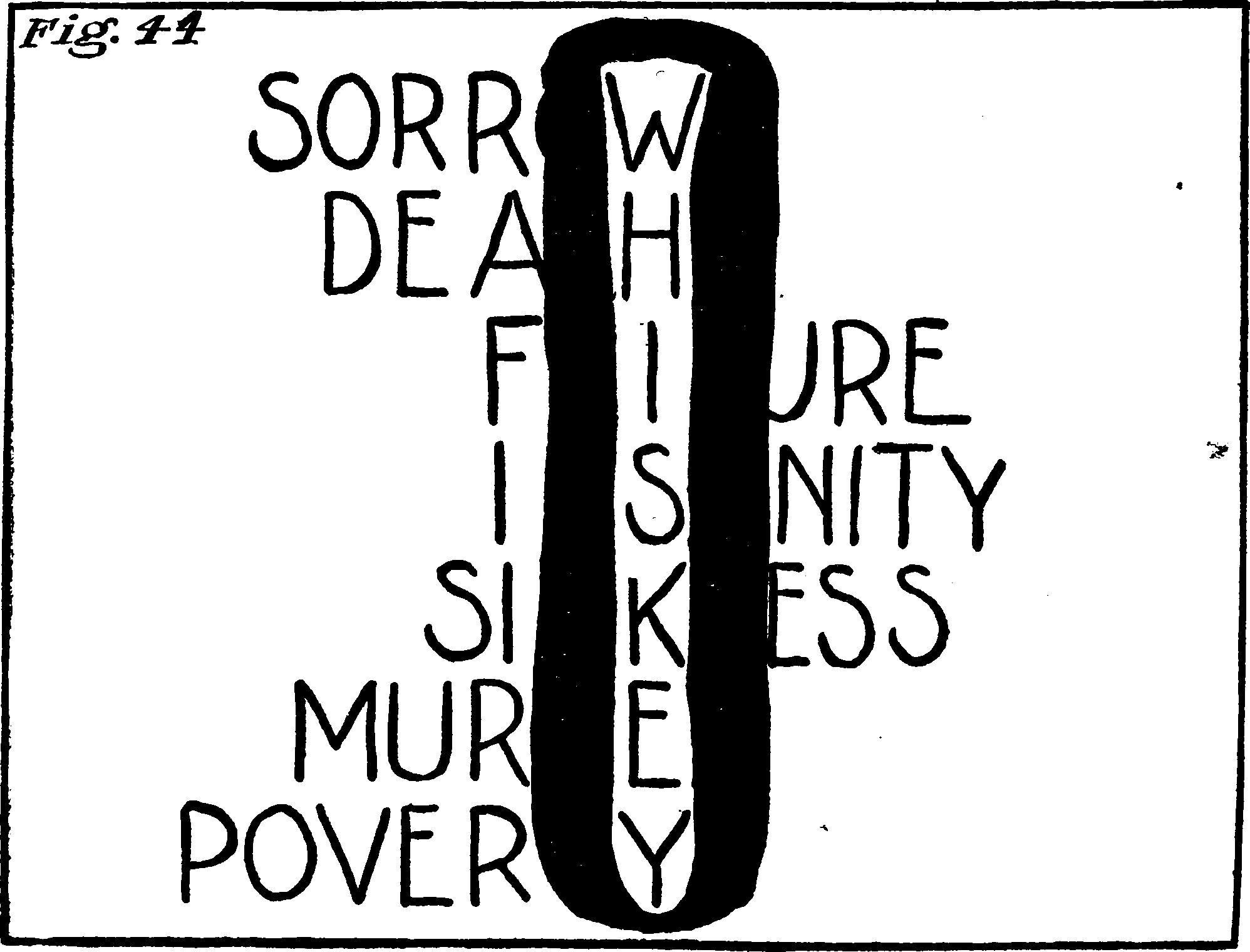
2.2 Self-fulfilling depression agendas
Or, as I now call them myths. This kind of thing:
Life gave me lemons and I have an amazing lemonade recipe but actually these are citrus limoni and taste better with citrus latifolia so there is no point in making it I would only be thinking about superior lemonades I cannot be making.
I do have ongoing questions about how to deal with the circular logic that depressed people seem to be especially likely to exhibit; I have noticed that someone who is really deep in will tend to construct a thicket of reasons to justify why the particular hole they are in is inescapable, and will grow new clauses justifying continued inaction, as each potential solution arises for the old problem. I am sad because no one wants to talk to me / No one wants to talk to me because I seem boring / thank you for offering to help facilitate a less boring conversation but actually I don’t want to talk to those people because actually it is they who are boring / thank you for offering to help me visit someone who I have previously said is not boring, but actually the weather is bad so I wouldn’t enjoy it… There are many versions of this.
When someone is depressed enough, they can always find a reason to avoid collecting evidence about whether certain things can alleviate what they claim is a direct stressor. A particularly smart depressed person might spend what looks to me to be considerable cognitive effort on finding an explanation as for why they cannot spend effort on things that look prima facie pretty useful, and why all the various solutions that arise are not quite right, and therefore pointless to try. I suspect this one would make more sense to me if I had suffered from more depression and I might learn how it is that, e.g. that talking about how stuff is terrible in a dark room is a free action, but talking about how stuff is terrible in the sunshine is gruelling.
Anyway, aside from my venting… Is it better to continue to attempt to refute such reasoning clause by clause, or does that lead only further into the sadness labyrinth?
The inactivity rationalization spiral is self-refuting. If you run far enough along a branch you will eventually find that the initial solution has been retconned out of existence. Perhaps running down these paths at all is destructive and is just helping the depressed person to eliminate choices from their life by publicly rejecting them, and then feeling compelled to stand by their reaxiomatization of the problem.
Would love hot tips on this.
3 Treatments
Exercise, sunlight, sleep but not too much apparently?
3.1 Pharmaceutical
- Scott Alexander, Peer Review Request: Ketamine
- My Experience with Ketamine for Depression
See also traditionally-recreational drugs in psychiatric care.
TODO: what is the state of evidence on psilocybin for depression? (Vargas et al. 2020; Carhart-Harris et al. 2016; Goldberg et al. 2020)
3.2 Sleep deprivation
Really. Guzey, in his review of sleep research mentions the following quote from somewhere(?)
Jeremy Hadfield writes:
My (summarised/simplified) hypothesis based on what I’ve read: depression involves rigid, non-flexible brain states that correspond to rigid depressive world models. Depression also involves a non-updating of models or inability to draw new connections (brain is even literally slightly lighter in depressed patients). Sleep involves revising/simplifying world models based on connections learned during the day, involves pruning unneeded or irrelevant synaptic connections. Thus, excessive sleep + depression = even less world model updating, even more rigid brain, even fewer new connections. Sleep deprivation can resolve this problem at least temporarily by ensuring that you stay awake for longer and keep adding connections, thus compensating for the decreased connection-building caused by depression and “forcing” a brain update.
4 What is depression actually?
- Once again, Scott Alexander, Peer Review Request: Depression
- I also think his Trapped Priors As A Basic Problem Of Rationality observation pertains here; see canalization.
- Motivated Reasoning As Mis-applied Reinforcement Learning
Guzey argues for a deeper connection with sleep.
Question: Does the dark room problem have anything to say about this?
5 Maintaining your own mental health around a depressed person
6 Incoming
Alexey Guzey, My journal: years of depression and self-loathing; learning to accept myself and others; overcoming video game addiction
Moncrieff in interview Lead author on that controversial new “depression not from serotonin imbalance” paper (Moncrieff et al. 2022; Read and Moncrieff 2022) in interview. TBH she lost me in the middle when she seemed to be basically denying that any drug could count as a productive input to the human experience ever.
How I Attained Persistent Self-Love, or, I Demand Deep Okayness For Everyone
Deep Okayness is not the feeling that I am awesome all the time. Instead, it is the total banishment of self-loathing. It is the deactivation of the part of my mind that used to attack itself. It’s the closure of the self as an attack surface. It’s the intuitive understanding that I am merely one of the apertures through which the universe expresses itself, so why would I hate that? It’s the sense that, while I might fuck up, my basic worth is beyond question—I have no essential damage, I am not polluted, I am fine … Our current thinking around mental health is broken. The dominant paradigm, as far as I can tell, is that you’re basically either unwell or you’re okay, and our job is triage. …
I would like to replace it with the following paradigm. There is a spectrum of background mental states, from “suicidal/dissociated/freaked out” to “abiding peace, happiness, and energy.” Nearly everyone can get pretty far up that spectrum. Nearly everyone can experience profound healing and become thoroughly Okay. It is your birthright.
Getting up that spectrum, and staying there, can be accomplished with a number of different psychotechnologies. A psychotechnology is anything that can alter your relationship with self, from mainstream talk therapy, to all kinds of meditation, to well-applied hallucinogens, to newfangled forms of therapy like IFS, etcetera.
Slate Star Codex, What Is Depression, Anyway?: The Synapse Hypothesis
Slate Star Codex, Things That Sometimes Help If You Have Depression
7 References
Footnotes
I am hoping this is not a causal relationship.↩︎